What is Dysphagia?
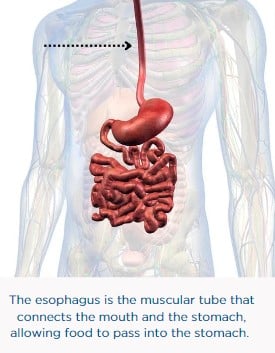
Dysphagia occurs when someone has difficulty swallowing. This can include feeling like solid or liquid foods are sticking, or not passing correctly through the esophagus. There are two types of dysphagia, each named to match the area of the esophagus affected.
- Oropharyngeal dysphagia occurs in the top of the throat behind the mouth. Patients with PD most commonly experience symptoms of oropharyngeal dysphagia.
- Esophageal dysphagia occurs only in the esophagus.
Parkinson’s disease (PD) and Dysphagia Together
Dysphagia likely happens in people with PD due to poor muscle movements. Muscles in the upper gastrointestinal (GI) tract may not move properly as a result of the affect PD has on muscles. For dysphagia to occur, the muscles in the esophagus may not contract as strongly, quickly, or in an organized way.
Research studies have shown that 35-80% of people with PD have dysphagia.
The relationship between PD and dysphagia may be caused by changes in the chemical signaling between the GI tract and the central nervous system (brain and spinal cord). This signaling is the way the body allows the brain and GI tract to communicate with each other. The muscle movements may slow down or occur out of their normal rhythm as a result. Changes in muscle movements are common throughout many parts of the body for people with PD, including the GI tract.
Learn more about Parkinson’s Disease and GI motility
Symptoms of Dysphagia
The symptoms of dysphagia depend on the area of the GI tract that is affected. The following symptoms may be seen in all people with dysphagia and include, but are not limited to, those who also have PD.
Oropharyngeal Dysphagia
- Difficulty starting to swallow, or being unable to properly swallow foods or liquids
- Coughing and choking – especially with eating or drinking
Esophageal Dysphagia
- Regurgitation – bringing food back up, this can sometimes occur through the nose
- A feeling that food is stuck in the throat
- Reflux – a burning feeling in the chest, especially the esophagus
Diagnosing Dysphagia
The following tests may be used to diagnose dysphagia in all people. People with Parkinson’s disease (PD) who are being tested for dysphagia will need to openly talk about all symptoms and health conditions with their healthcare provider. This allows them to decide the safest and most effective testing option for each person.
- Pharyngeal high-resolution manometry (HRM) – A thin tube is placed in the nose and through the throat and esophagus. Patients then swallow small sips of water while the tube measures the pressure created by each swallow.
- Videofluoroscopy – This test involves a moving x-ray that allows a healthcare provider to watch swallowing as it is happening.
- Barium swallow – After drinking a liquid containing barium, an x-ray is used to watch and take pictures of the flow of the liquid through the esophagus. Barium is an element that is slightly radioactive, making it safe and effective for use with x-ray tests.
- Flexible endoscopic evaluation of swallowing – A camera is attached on the end of a long, flexible tube with a camera and light on the end. It is placed into the nose and travels down the esophagus. This test allows your healthcare provider to see inside your GI tract during the test, so they can see swallowing as it occurs.
Treatment Options
The treatment options listed below may be used in all people with dysphagia, including those who are living with Parkinson’s disease (PD).
Treatment options are dependent on what will best meet the needs of each individual. This can include more options than are provided in this article.
- Botulinum toxin type A – This may be injected into the muscles connecting the esophagus and stomach (gastroesophageal sphincter). Botulinum is a toxin produced by bacteria that can be used as a treatment to block nerves and muscles from communicating with each other.
- Dopamine agonists (such as ropinirole and apomorphine) – This type of medicine mimics dopamine and turns on dopamine receptors. This tricks the brain into thinking there is enough dopamine in the body, which can improve some symptoms.
- Rehabilitation – This can include swallowing behavioral therapy and speech pathology to help train the muscles and improve swallowing.
Adapted from IFFGD publication #405 “Parkinson’s Disease (PD) and Dysphagia” by Baharak Moshiree MD MSc, Mackenzie Jarvis PA-C, DMs, Atrium Health, Wake Forest, Digestive Health-Morehead Medical Plaza; Marissa Lombardi, International Foundation for Gastrointestinal Disorders










